Appraisal Considerations Shifting as COVID-19 Disrupts Health Care Delivery

In this article, we examine how the COVID-19 pandemic is reshaping the configuration of critical and other care facilities, and what that is likely to mean for hospitals and the broader health care real estate market moving forward.
Innovation in health care delivery has lagged behind the speed with which many other industries have experienced change in recent years. In a 2019 article, HealthManagement.org put it this way, “No other industry that operates as inefficiently and ineffectively as health care has survived disruption in the 21st century.” Given its singlehanded and rapid impact on supply chains, large enterprises, small businesses and the health care industry itself, COVID-19 can, in many ways, be considered the ultimate disruptor. So, has the industry finally met its match?
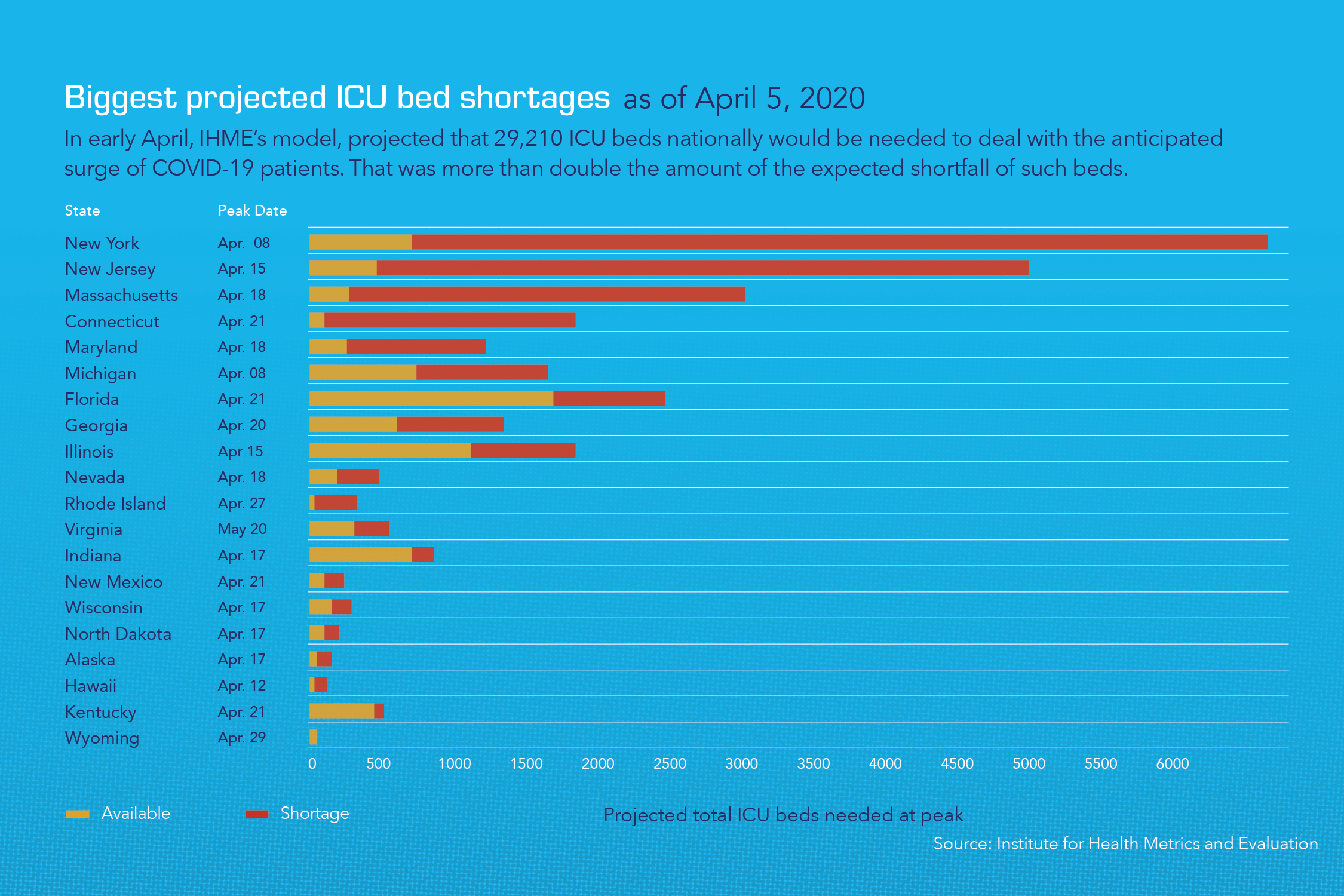
In light of COVID-19, health care systems are facing unprecedented headwinds in respect to both current and future regulations for designation of virus treatment and elective care areas. The emergency processes and revised configurations quickly put into place for managing patient care as the current crisis has unfolded will likely evolve into a series of future organizational and facilities planning requirements/best practices that will alter how patient care is delivered moving ahead. It may well become a requirement, for example, for urgent care providers to have facilities that isolate onboarding treatment areas, which will result in the need to modify floor designs, rendering many existing facilities sub-optimal for that purpose. Similarly, ICU’s might be required to have built-in flexibility allowing for their rapid mobilization and conversion to expandable quarantine areas with a separate drop-off and entry point. In some cases, this may also require the use of separate and distinct medical facilities for that purpose. We believe that this, in turn, is likely to result in increased efforts to readapt existing uses in order to deliver the specific types of care in the manner required.
At the same time, the current crisis has also intensified an overall focus on both antiquated and shuttered medical facilities nationwide and the best future use of these structures and their associated real estate. Beyond regulatory factors, evolutionary changes in the industry, such as providers’ accelerated ramp-up of telemedicine during the pandemic period, may impact real estate footprint needs in the long term. Other learnings from operational changes made during this time, including successful execution of remote administrative and back-office functions by personnel mandated to work remotely, may also enter into this equation.
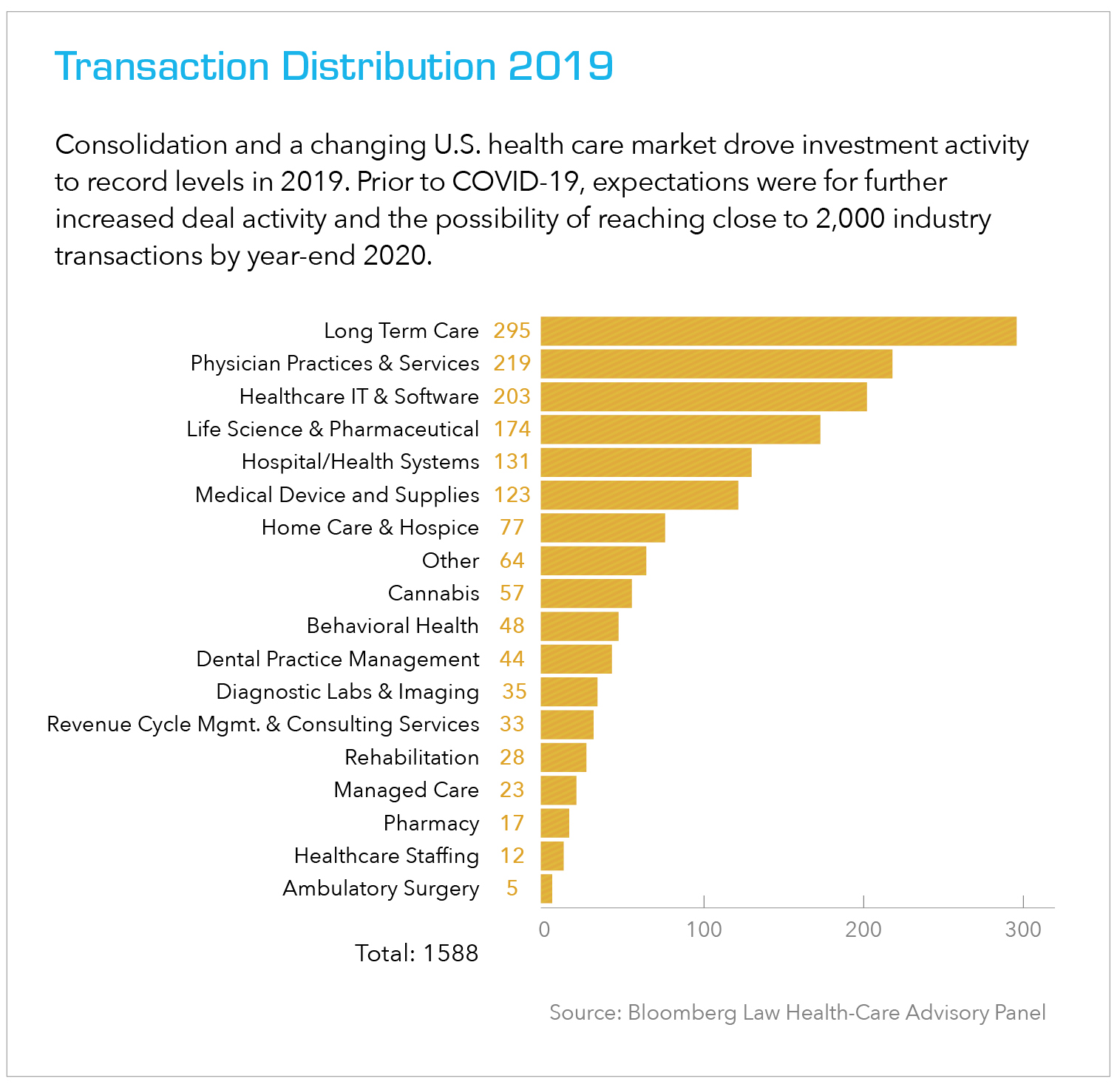
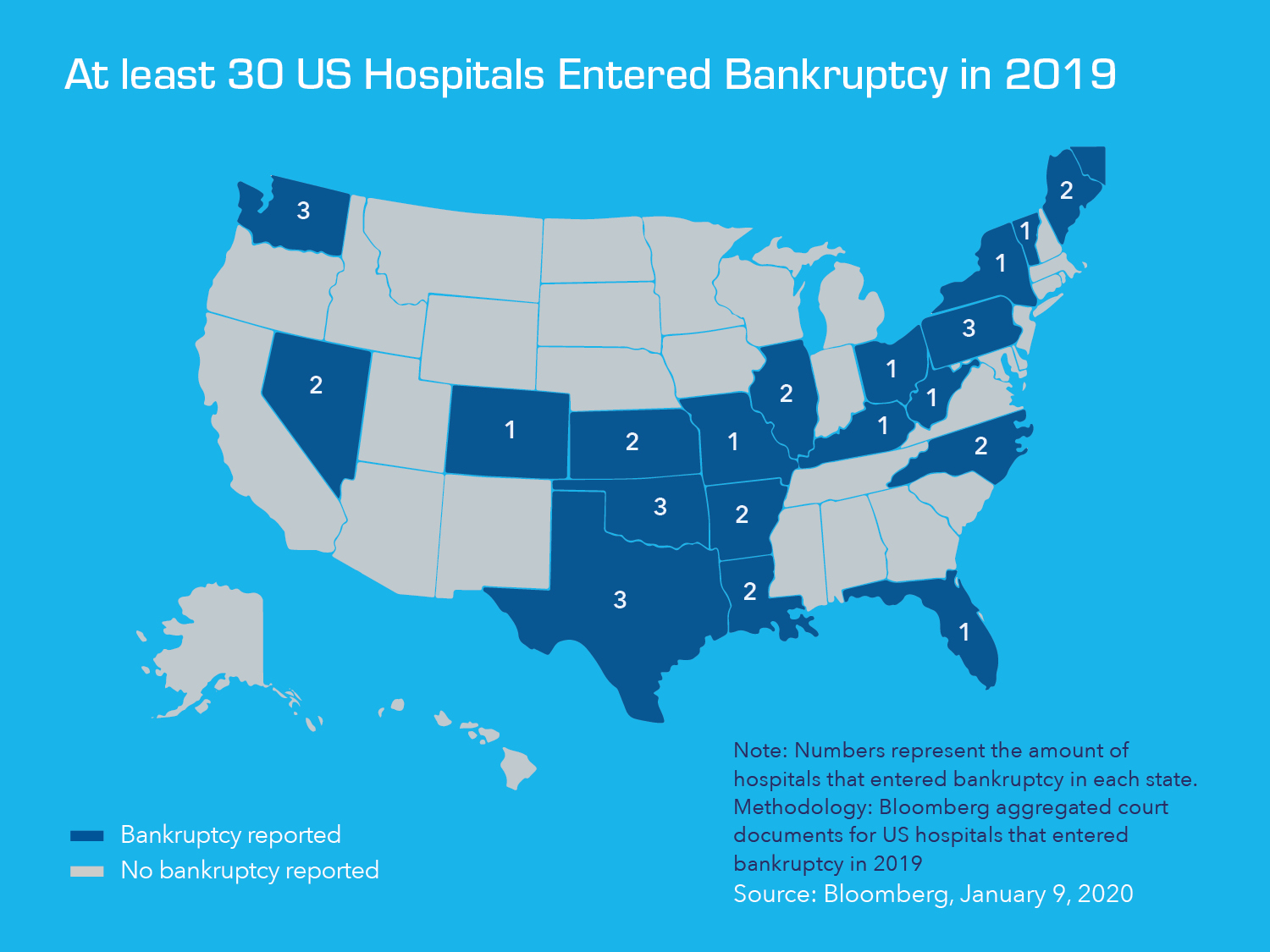
Leading into 2020, with the health care market continuing to undergo transition in terms of where and how its services are delivered, a notable number of hospitals and the hospital systems which operate them across the U.S., were finding themselves in somewhat unfamiliar territory. As the pace of consolidation between and within hospital systems has quickened in recent years, more and more providers overall have been looking to reassess and refocus their care delivery strategies. As a result, we have seen a notable increase in the number of underutilized and shuttered hospitals nationwide.
These developments are being driven by a variety of factors including an increased emphasis on highly proactive, continuous wellness programs as well as shifting population and urban gentrification trends. As Gensler Research & Insight explains it, “These are the hospitals left behind, and the phenomenon only promises to grow. The question of what to do with underutilized or closed hospital buildings is of vital importance, not only to the buildings’ owners and operators, but to the patients and communities they were built to serve.”
While many aspects of the health care experience have been automated or made accessible via the online/mobile experience in recent years, for the most part – virtual appointments aside – the delivery of care is still predominantly conducted at physical locations that house medical personnel and the vast array of diagnostic and other equipment needed to fulfil the needs of patients. This is true for aging facilities as well as for new locations designed to meet the changing needs of today’s patient populations. The key difference is the mix of services delivered and the configuration of space required to do so today vs. in the past.
To maximize the efficient use of both physical and human capital while best serving patients where they live and work, satellite facilities have proliferated in recent years. While provider execution may vary to some degree, the principles of centralization, itself, within health care are relatively consistent. Typically, this has involved use of a main campus supported by satellite locations dispersed geographically based upon an assessment of market need and projected revenue, among other considerations. The main/centralized facility handles the vast majority of critical care needs and houses the many back-office functions such as HR, IT, etc. A host of other care services are then delivered across the satellite network, providing greater ease of access to the patients and efficiencies for the system. When a level of care that exceeds the scope of a satellite location’s services is needed, patients can be referred either to another specialty satellite facility or to the main hospital setting for delivery of more complex, critical or highly technical care.
The current environment, however, is anything but typical. While consolidation or closure of newer or more recently modernized hospitals for strategic purposes creates opportunities for retrofitting existing spaces within those facilities to suit current needs, pre-pandemic and pandemic period thinking are likely to diverge on the best use of those spaces. Before COVID-19, prevailing thought might have been to repurpose spaces that previously served as ERs into urgent care centers, and those that were ORs into surgi-centers. Moving forward, that may not be the case, although our view is that there will most certainly be scenarios where it still makes sense to repurpose an entire facility to serve in a specialty capacity such as an orthopedics or drug rehabilitation campus.
When built, many older hospitals in urban areas were strategically located with public transportation in mind. That proximity to train and bus routes makes them, or in some cases just their real estate, highly desirable today for reconfiguration or redevelopment as residential or other properties. Whether a facility is newer or older, in transition or shuttered altogether, it is critical to carefully examine all underlying assets associated with the target property to achieve the best possible valuation and make a truly informed decision as to a course of action.
Obstacles
Pandemic considerations aside, there always have been, and will continue to be, numerous potential obstacles to determining the highest and best use/reuse of hospitals, health care facilities and their associated real estate. These may include factors such as the limitations of the existing physical structure that occupies the real estate, the way it was constructed initially, the level of decay, the cost of remediation or other physical factors.
Additionally, the interest and influence of stakeholders within the community cannot be underestimated. Many projects have derailed when members of the immediate and nearby communities were not “heard” or on-board. This can range from a strong presence at community meetings to discuss the project, to public protests, aggressive lobbying and use of news media. Foregoing a project due to community resistance is highly undesirable, particularly when other hurdles have been overcome.
Often times the dissatisfaction stems from the fact that the proposed reuse is far removed from the original use or even the reuse that was initially proposed but altered due to diligence, economic, or other realities. The bottom line is usually, if stakeholders don’t share the vision that the new proposed use will benefit the community, or worse, will do the community a disservice- its chances of successful support by community members and local political and other influencers is highly unlikely.
The conversion of a property from one approved use to another will most certainly require zoning approval and may also entail reviews from appearance and other boards as well as local and/or state regulatory bodies. This is not surprising, particularly when the new use will be distinctly unique from the original, approved use. Hilco is expert at the diligence required to determine the scope, timing and other impacts posed by these and the other types of approvals needed to ensure a project’s success.
Determining Future Uses
Adaptive Reuse:
Our real estate appraisal team has deep expertise in interpreting the trend line for the transition of an existing hospital or health care facility from one purpose to another, including factors such as the potential end use tenant profile and income stream, and how to value the transition from what might now be an obsolete or vacant facility into what will become a dynamic repurposed use.
Understanding underutilized assets and how to value them based on how they can be used in the market within the health care space is a Hilco sweet spot. In some cases, we are approached by a property owner or provider directly. In others, we are sought out by private equity investors and collateral-backed lenders interested in providing construction-to-permanent financing or other capital for tenant improvements related to an adaptive reuse. In each instance, we look at these engagements holistically to understand and define the market, the target users, target rent and factors such as the absorption rate and tenant mix vision.
A functioning hospital, for example is valued as an enterprise (going concern) in its entirety, so among other things we will assess EBITDA and then utilize either an income, sales comparison or cost approach in our analysis to break out residual business value, real estate and FF&E or all tangible and intangible components.
Demolition & Redevelopment:
While in some cases, we are engaged to provide a valuation of the underlying real estate assets only, we are often asked to both evaluate those assets and to provide an assessment of their highest and best future use. This is frequently the case when a hospital has been acquired by a larger system and although it remains in operation, it is highly underutilized or no longer likely viable as a going concern. This can be the result of the “satellite” phenomenon described earlier or may, among other factors, be a consequence of serving a community with a high level of Medicaid and Medicare recipient patients, where slow payment by the state has resulted in a significant backlog of receivables. In these situations, the owners may seek the valuation to help determine what it might be able to capture in a line of credit against those assets. A bank, in turn, may seek its own valuation to justify granting that line.
In instances such as these, Hilco will focus on valuing the land and associated buildings/structures on behalf of the owners or bank, taking into account any current or potential use of those as part of the valuation process. We will run models to test for potential market acceptance of the asset as a continued going concern hospital. If there is no tangible brand or enterprise value given the entity’s position in the market, then oftentimes the recommendation may be for redevelopment.
Partial Demolition/Services Consolidation:
Some facilities across the country, particularly those of long-standing providers in urban neighborhoods dating back to the earlier 1900s, have found themselves squarely in the path of redevelopment. Circumstances such as these can present significant opportunities, but also involve certain challenges as well. We have worked with some hospitals in this situation, for example, that are not viable entities or have only been able to remain open due to the generosity of waning private donations. In many cases, we have seen facilities that are wholly antiquated or are operating a single, more modern wing while the remainder of the original structures on the property have been shuttered. One complication we encounter with some regularity here is an encumbrance on highest and best use/redevelopment based on a hospital’s designation as a high trauma center, with the state requiring it to remain in place as a community asset. In our experience, facilities such as these have proven to be good targets for hybrid redevelopment, with a percentage of the functional property remaining in place, while the remainder is razed for another suitable use and any satellite facilities are sold off.
In Summary
The COVID-19 crisis will unquestionably play a large role in shaping the future of hospital design, care and investment. Federal and state regulatory requirements are likely to mandate upgrades to facilities that enable – among other capabilities – rapid flexing of emergency room and isolation areas. In many cases, the physical limitations of aging facilities may be a barrier to meeting these requirements. Additionally, with many voices during the current crisis calling for a commitment to increase the overall number of hospital beds nationwide, while others suggest a “hospital at home” solution to transform mild or moderately ill patients’ own residential beds into hospital beds when future crises strike… the hospital landscape is certain to experience disruptive change.
During the current crisis, we are having numerous conversations across the industry and are actively working with both lenders who have hospital portfolio exposure, as well as with operators interested in understanding monetizing options for their assets. By leveraging our expertise and proprietary industry lifecycle analysis and data, we are assisting them with immediate valuation modeling as well as to better understand and plan for what comes next through the current market cycle. Whether your assets are healthy functioning entities or near distress, we can help you recognize value trends in the market, capitalize on timely opportunities and avoid potentially costly missteps. Give us a call. We are here to help!



